MRI Fusion Trans-perineal Prostate Biopsies under General Anaesthesia
This leaflet contains evidence-based information “MRI Fusion Trans-perineal Prostate Biopsies”. Although we have consulted specialist surgeons and practitioners during its preparation, most of the content is adapted from the British Association of Urological Surgeons (BAUS); so that it represents best practice in UK urology. You should use this leaflet in addition to any advice already given to you.
This leaflet contains evidence-based information “MRI Fusion Trans-perineal Prostate Biopsies”. Although we have consulted specialist surgeons and practitioners during its preparation, most of the content is adapted from the British Association of Urological Surgeons (BAUS); so that it represents best practice in UK urology. You should use this leaflet in addition to any advice already given to you.
Key points
|
Do I need any preparation?
While your procedure will be carried out under general anaesthetic, you need to fast for six hours prior to the procedure. You can drink water up-to 2 hours prior to the procedure. You need to take your prescription medication as usual. If you are on any anti-coagulant medication (blood thinning medication), please inform your urologist and seek further advice. Our preoperative assessment team will further advice you on this.
What does this procedure involve?
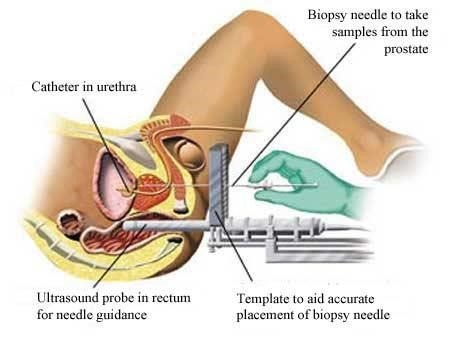
The procedure will be performed under general anaesthetic, in one of our minor operations room. The procedure involves putting an ultrasound probe into your rectum (back passage) to scan your prostate. Guided by ultrasound and prostate MRI images, biopsies are taken from your prostate through your perineum (the skin between your scrotum and rectum).
What are the alternatives?
- Observation with repeat blood tests & Prostate MRI – repeating your blood tests and only investigating further if you PSA (prostate specific antigen) levels rise.
What happens on the day of the procedure?
A member of the urology team will give you a container for a urine sample to test for infections. They will also measure and record your vital signs: blood pressure, heart rate, oxygen saturation, and temperature.
You will be reviewed by our anaesthetist.
Your urologist (or a member of their team) will briefly review your history and medications, and will discuss the procedure again with you to confirm your consent.
Details of the procedure
- Before the procedure, we will give you an antibiotic injection, after we have checked carefully for any allergies
- We position you in special supports which allow the surgeon to access the skin behind your scrotum
- We will use an antiseptic solution to clean your perineum
- We than insert an ultrasound probe into your back passage to scan your prostate. An advanced software package (MRI fusion) is used to take targeted samples from high risk areas identified on the MRI images. This ensure that the samples can be taken with great precision.
- The biopsy needles are guided into position using the ultrasound scanner (pictured) and the MRI Fusion software.
- The number of biopsies taken depends on your PSA level, the MRI report and other risk factors
- We apply a dressing to your perineum.
- The procedure takes 25 to 30 minutes to complete
- You should expect to go home after couple of hours of the procedure
Are there any after-effects?
The possible after-effects and your risk of getting them are shown below. Some are self-limiting or reversible, but others are not. The impact of these after-effects can vary a lot from patient to patient; you should ask your surgeon’s advice about the risks and their impact on you as an individual:
| After-effect | Risk |
| Blood in your urine for up to 10 days | Almost all patients |
| Blood in your semen which can last up to six weeks (this poses no risk to you or your sexual partner) | Almost all patients |
| Bruising in your perineal area (space between your testicles and back passage). | Between 1 in 2 & 1 in 10 patients |
| Discomfort in your prostate caused by bruising from the biopsies | Between 1 in 2 & 1 in 10 patients |
| Temporary problems with erections caused by bruising from the biopsies | 1 in 20 patients (5%) |
| Inability to pass urine (acute retention of urine) | 1 in 20 patients (5%) |
| Bleeding in your urine preventing you from passing urine (clot retention) | 1 in 50 patients (2%) |
| Failure to detect a significant cancer in your prostate | Between 1 in 10 & 1 in 50 patients |
| Need for a repeat procedure if biopsies are inconclusive or your PSA level rises further | Between 1 in 10 & 1 in 50 patients |
| Bleeding in your urine requiring emergency admission for treatment | 1 in 100 patients (1%) |
| Infection in your urine requiring antibiotics | 1 in 100 patients (1%) |
| Septicaemia (blood infection) requiring emergency admission for treatment | Less than 1 in 100 patients (<1%) |
What is my risk of a hospital-acquired infection?
Your risk of getting an infection in hospital is between 4 & 6%; this includes getting MRSA or a Clostridium difficile bowel infection. This figure is lower for a day-case admission but higher in a group of patients who have had:
- long-term drainage tubes (e.g. catheters);
- long hospital stays; or
- multiple hospital admissions.
What can I expect when I get home?
- We advise you to drink plenty of fluid (up to 2 litres of water) per day for 3-4 days.
- you will be given advice about your recovery at home
- you will be given a copy of your discharge summary if the procedure is performed under general anaesthetic and a copy will also be sent to your GP
- you will be given 2 doses of antibiotics to take home
- if the bleeding in your urine does not stop, you should contact your GP or specialist nurse or report to nearest accident and emergency.
- if you are unable to pass urine at all, you should contact your GP immediately or go to your local Emergency Department
- we will review the results of your biopsies in a multidisciplinary team (MDT) meeting within three weeks. The MDT comprises of urologist, oncologists, radiologists and histopathologists.
General information about surgical procedures
Before your procedure
Please tell a member of the medical team if you have:
- an implanted foreign body (stent, joint replacement, pacemaker, heart valve, blood vessel graft);
- a regular prescription for a blood thinning agent (e.g. warfarin, aspirin, clopidogrel, rivaroxaban, dabigatran);
- a present or previous MRSA infection; or
- a high risk of variant-CJD (e.g. if you have had a corneal transplant, a neurosurgical dural transplant or human growth hormone treatment).
Smoking and surgery
Ideally, we would prefer you to stop smoking before any procedure. Smoking can worsen some urological conditions and makes complications more likely after surgery. For advice on stopping, you can:
- contact your GP;
- access your local NHS Smoking Help Online; or
- ring the free NHS Smoking Helpline on 0300 123 1044.
Driving after surgery
It is your responsibility to make sure you are fit to drive after any surgical procedure. You only need to contact the DVLA if your ability to drive is likely to be affected for more than three months. If it is, you should check with your insurance company before driving again.

