Home parenteral nutrition for children
Your child has been diagnosed with Intestinal Failure and therefore requires Home Parenteral Nutrition (HPN), to meet their nutritional needs. There are many condition’s that can lead to Intestinal Failure, your child’s diagnosis will be discussed and explained to you by the Nutrition Team.
Childs Name:____________________________________
Diagnosis (including bowel length):____________________________________
Paediatric core nutrition team:
- Dr Krishna Soondrum- Consultant Paediatric Gastroenterologist
- Danielle Ellis- Paediatric Nutrition Clinical Nurse Specialist
- Piya Dhulia- Paediatric PN Pharmacist
- Charlene Chavda- Paediatric PN Pharmacist
- Sophie Daborn- Specialist Paediatric GI Dietician
Expanded multidisciplinary team:
- Drs Fell, Epstein and Thangarajah- Consultant Paediatric Gastroenterologists
- Mr Simon Clarke- Consultant Paediatric Surgeon
- Lisa Davey- Clinical Nurse Specialist Paediatric IBD
- Jackie Falconer and Bonnie Samani- Specialist Paediatric GI Dieticians
- Simone Hunt- Mercury Ward Manager
- Mercury Ward Nurses
- Amy and Gitta- Play team
- Samanthi Perera-Gill- Clinical Psychologist
- Drs Ben Roberton and Brahman D- Interventional Radiologists
- Laura and Analou- Speech and Language Therapists
What Is Parenteral Nutrition (PN)?
Parenteral Nutrition (PN) is used when the digestive tract is unable to absorb enough fluid, energy and nutrients.
Parenteral Nutrition is delivered directly into the bloodstream, where the body can easily absorb and use it for energy, growth and development.
Parenteral Nutrition contains lots of ingredients:
- Water – Sterile Water is used in PN to prevent dehydration.
- Carbohydrates – These are the calories that provide the body with energy.
- Fat (Lipids) – Are another source of calories and energy.
- Protein (Nitrogen) – Is really important for growth and repair in the body. Protein also plays an important part in helping the body fight infection and the healing process
- Vitamins – Each Vitamin has a different job to do in the body. They are essential in keeping the body healthy and to grow normally.
- Minerals (Electrolytes) – The minerals that we talk about more often are Sodium, Potassium, Calcium, Phosphate and Magnesium. They help build a strong skeleton and are used by the nerves and muscles in our body.
- Trace Elements – These are also minerals – but we don’t need as much of these in our body. They include Zinc, Copper, Magnesium and Selenium.
Everyone will have different nutritional requirements; therefore every child needs a different recipe. Every recipe (prescription) is calculated by the specialist nutrition team for your child. Once the prescription has been finalised, the PN is made in a compounding unit (a sterile environment) and will be delivered to you in bags that are ready to be used.
This prescription can change over time depending on your child’s growth, age and if they are managing to tolerate enteral/oral feeds.
How do we deliver PN into the blood stream?
Home Parenteral Nutrition is delivered into the blood stream via a Central Venous Line (CVL). A central venous line sits in a central vein, close to the heart. This allows for the PN to be administered and circulated into the body quickly and safely.
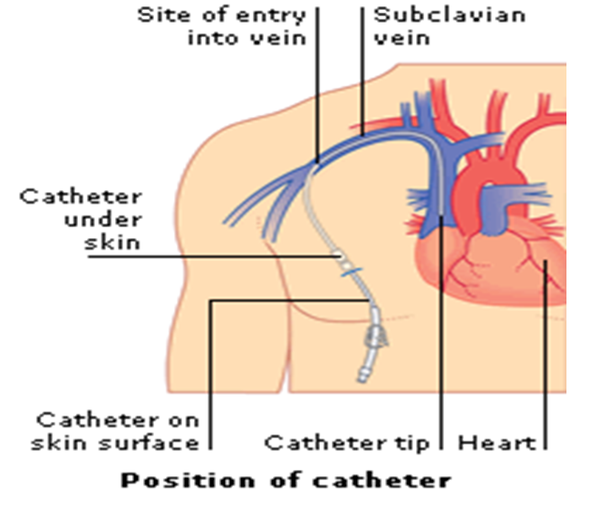
Central Venous Lines can be inserted in Interventional Radiology and sometimes in a theatre (surgery). The central line is inserted into a vein through an incision (small cut) made around the level of the collarbone. The tip (end) is threaded through and sits in a large vein that leads to the top of the heart.
The other end that you can see is tunnelled under the skin and comes out generally on the chest area – called the exit site. For all children this procedure is completed under a general anaesthetic.
Date Central Line Inserted:___________________
Central Line Size:___________________
Central Line Position:___________________
Central venous line safety
The central line has various parts which you need to recognise:
The Dacron Cuff – this should not normally be visible. This is a special sleeve which surrounds the line underneath the skin at the place where the line enters the chest (the exit site). The Dacron Cuff is made of a special material, which adheres to the tissue to prevent the line from falling out and helps to prevent infection. When the line is put in it may take some time for the Dacron Cuff to adhere to the tissue. If at any point you can see the Dacron Cuff this means that the line must have moved and will need to be checked before you use it.
The Dressing and Exit Site – the central line should always have a dressing to cover the exit site (where the central line leaves the body). Underneath the dressing the central line must always be positioned with at least one loop. Most of the time, the dressing will be occlusive (see through) so that you can see the exit site and the loop under the dressing. The dressing must be changed at least once a week.
The Clamp – is situated above the hub and is used as a safety device to prevent the flow of any fluid, air or blood into or out of the line. The clamp should be placed on the thicker reinforced area of the line. This is designed to stop the clamp from damaging the line itself. There may be times when you need to clamp the line close to your child’s chest – this will not be possible if your child has a multi lumen line, or if the clamp is faulty. You must ensure that your child’s emergency pack with disposable blue clamps is with you at all times.
The Hub – is the hard plastic portion at the end of the line, (usually red or white in colour), which is used to access the line. The Hub should always have a Bionector attached to it as a safety mechanism. When the line is not in use the Bionector should be covered with a port protector (Parafilm).
Bionectors - are ‘needle-less’, ‘closed – system’ devices. They enable you to access the central line, without ever exposing the inside of it. A Bionector can be used to give drugs or flushes by bolus or infusion or in order to take blood. A Bionector has a built in valve, which remains closed unless you attach a syringe or giving set to it. A Bionector must be changed once a week, for this reason many people choose to do this after they have completed the weekly central line dressing.
The Port Protector – a disposable passive disinfection device. This is used to reduce central line infections by keeping the Bionector clean when not in use. This is disposable – every time the central line is disconnected a new device is used. If the line is not in use they can remain in situ for seven days.
Name and size of the dressing you/your child is using:________________________
Central line safety advice including daily care and observations
Infection
Central Venous Line Infections are one of the most serious and potentially life threatening complications that can happen. As well as the most serious, a central line infection is one of the most frequent complications that we see. It is therefore essential that all precautions are taken to try and reduce and eradicate the chance of infection.
Please note that if your child develops a temperature of 38degrees and above you should do to your local hospital immediately as your child could have a line infection or sepsis.
If worried or unsure please ring 999 and ask for an ambulance to take you to your local hospital.
- Observe the exit site and neck wound for any signs of infection;
- Redness
- Swelling
- Pain
- Heat
- Discharge i.e. blood/pus
Should any of the above occur please take your child to their local hospital or call your community nurse for assessment. Your child will require an assessment, swabs and blood specimens to be taken.
- If the central line is infected then it will need prompt treatment.
- If the dressing is soiled with blood or there is wetness under the dressing it will need to be changed as this increases the risk of infection.
- If the dressing remains intact and there is no oozing then the dressing needs to be changed once a week by the children’s’ community team.
When can I given paracetamol to my child?
Never give Paracetamol to treat a temperature. You may want to give Paracetamol/Calpol as pain relief. If using Paracetamol to treat pain, please do not give it for two hours before the PN starts and for two hours after it has started OR within two hours of the PN completion and for two after the PN has been disconnected. These are the times that are higher risk and therefore we do not want to hide a temperature. If you are ever unsure, please just call us to check.
Emergency central line care
Prevention
- Always ensure that your child’s dressing is secure and intact.
- The dressing must include a loop in the central venous line.
- Ensure that the clamp is closed when the infusion has been discontinued.
- Observe the central line site for any signs of infection (red, pus, swelling, bleeding and broken skin). Any concerns please contact the nutrition team.
- Ensure that the Bionector is secure and in place. If the Bionector is missing you must replace this as a matter of urgency but with the correct technique. Never replace the dirty Bionector.
- Ensure that the port protector is in situ if the infusion has stopped.
- Always check your child’s central line and dressing is intact prior to leaving the home. Depending on the age of your child, they must also participate in these checks.
- Always ensure that you have an Emergency Central Line pack and a copy of the Hand Held letter with you at all times.
|
Problem |
Possible Cause |
Action |
Prevention |
|
Leak of blood and/or PN from Central Line |
Hole in the line |
If the PN is running, this needs to be stopped. If you can see the hole, wrap the area in sterile gauze and clamp just above the hole. Use the second clamp in the emergency pack to clamp as close to the dressing as possible (wrapping the clamp area with gauze). If you cannot see a hole, use both clamps and clamp using gauze, as close as you can to the dressing edge. Contact C&W and attend A&E. |
Good dressing and securement techniques. Use of ambulatory pumps. Risk assessment for environmental hazards |
|
Central Line break |
Central line has snapped in half due to repair or accident. |
If the PN is running, this needs to be stopped. If the clamp belonging to line remains in place – ensure it is clamped. Kink the end of the line, wrap in gauze and clamp the kink. Place the second clamp in the emergency pack at the edge of the dressing (using gauze) Contact C&W and attend A&E. |
Good dressing and securement techniques. Use of ambulatory pumps. Risk assessment for environmental hazards. After two breaks in the central line, a planned elective replacement will be organised. |
|
Redness, swelling, tenderness, pus or bleeding at the exit site. |
Possible site infection |
Contact the Nutrition team at C&W or Community Nursing Team. Swabs will be taken, topical treatment commenced and dressing technique changed to daily. |
Aseptic non touch technique. Weekly dressing changes. Quick recognition and treatment. |
|
Trauma, missing loop in the central line dressing, Dacron cuff visible externally |
Central line has been dislodged |
If the PN is running, this needs to be stopped. Leave the dressing in place. Take the long length of the central line and wrap above the exit site, on top of the dressing. Cover the bundle of line in gauze and secure with tape (all in the emergency kit) Contact C&W and attend A&E. |
Good dressing and securement techniques. Use of ambulatory pumps. Risk assessment for environmental hazards.
|
|
Central line has been accidentally removed |
Central line has been completely removed. |
Sit the child on your lap or next to you on a chair. Take the sterile gauze from the emergency pack, fold into four and place on the hole that the line came out from and apply pressure. Call 999 (remembering to state a central venous line has been pulled out). Keep applying new gauze when soaked with blood – NEVER remove the original placed gauze (this may remove and mechanism of blood clotting and increase bleeding). Try not to move the child – this may increase bleeding. |
Good dressing and securement techniques. Use of ambulatory pumps. Risk assessment for environmental hazards.
|
|
Chest Pain. Shortness of Breath. |
Possible Air Embolism |
Place the child onto their left hand side (if this is proving hard – cuddle them across your lap onto the left side – aiding reassurance. Call 999 remembering to state the symptoms and that the child has a central venous line. |
Ensure the Bionector is in situ at all times. Ensure the clamp is secure. Ensure all air is removed for syringes and giving sets prior to use. |
|
Feeling Unwell |
Possible Central Line Infection |
Follow the sepsis protocol. |
Aseptic non touch technique |
If you have needed to discontinue the PN mid infusion, remember there is a risk of low blood sugar. If your child receives an enteral feed continue or commence this. Encourage them to have a drink or eat what they can within their diet.
In an emergency, it is essential that you attend the nearest A&E – remembering to take your Hand Held letter. Let the Nutrition team know when and where you have been admitted.
You will be provided with a safety pack containing the following items:
- 1 x pack sterile gauze
- 1 x large IV 3000 dressing
- 1 x small IV 3000
- 2 x blue clamps
- 2 x bionectors
- 4 x sani cloth CHG 2%
- 1 x roll transpore
The safety kit should accompany the child at all times, anyone caring for the child must be familiar with the pack and must have received safety training.
Your home and parenteral nutrition
All patients that are discharged home with Parenteral Nutrition must have a home assessment. This is a national requirement to ensure that the environment is safe and that you have all that you will need before going home. We will help you decide where the connection/disconnection and care procedures would be best carried out and the options for storage of the ancillaries and equipment including a dedicated fridge.
Sometimes your home may need some rearranging – we can help to advise on this. For some people we need to explore housing options if the home does not have the capacity for a patient on home parenteral nutrition.
|
Yes/Comment |
No/Comment |
|
|
Adequate space for setting up HPN |
|
|
|
Adequate space for PN fridge- normal standard long fridge |
|
|
|
Adequate space for storage consumables – trolley, IV stand, Boxes e.t.c |
|
|
|
Number of steps into property |
|
|
|
Number of steps to bedroom |
|
|
|
Number of steps to location of fridge |
|
|
|
Close located hand washing sink |
|
|
|
Number power sockets |
|
|
|
Heating/Ventilation |
|
|
|
Cleanliness |
|
|
|
Pets |
|
|
|
Number of rooms |
|
|
|
Number of people living in the property |
|
|
|
Own home |
|
|
Home care companies and the National Home Parenteral Nutrition (HPN) framework.
The national HPN framework was commissioned by NHS England to improve standards and access to home parenteral nutrition services for adults and children in England. Only companies who have formally applied to be on the framework and have demonstrated they meet the specified standards are authorised to provide homecare.
The National Framework Agreement for the Supply of Home Parenteral Nutrition for England (or framework for short) covers all aspects of home parenteral nutrition, including the making and delivery of the feed and ancillaries, and the provision of specialist nursing for those not able to administer the feed themselves. It was developed as part of a national tender commissioned via NHS England and the Commercial Medicines Unit of the Department of Health.
When your child is nearly ready for discharge, the chosen home care company will conduct an installation visit to deliver and set up the larger pieces of equipment (including the fridge) and ancillaries. Once you are at home, the company will deliver your child’s PN – this is generally on a weekly or fortnightly basis depending upon the prescription. They will also deliver supplies of ancillaries – they will call you prior to a delivery to ask what you need.
The company will discuss your delivery day and time – you will be allocated a two hour delivery time slot. It is essential that someone is at home or that you have made, the necessary arrangements for someone to let the delivery driver in – the PN must be unpacked straight into the fridge.
You will be given contact details for your co-ordinator including an out of hour’s emergency telephone number.
If at any time you are unhappy with the home care company, please call us to chat through any concerns/problems.
Your Home Care Company is called _____________________________________
The contact number for your Home Care Company is ________________________
Your patient care co-ordinator is _________________________________________
How to store parenteral nutrition at home
The chosen home care company will deliver all of the equipment that you require for storing and administering Parenteral Nutrition in the home, during the installation visit.
You will be provided with a dedicated fridge to store the Parenteral Nutrition. This fridge will come equipped with a thermometer, so that you can monitor the storage temperature.
- The fridge MUST only ever be used to store the Parenteral Nutrition and for some people the central line locks. This fridge MUST never store food products or medicines that are given orally or enterally. This is also true if you go on holiday.
- The Parenteral nutrition bags must be stored in single layers on each shelf (no stacking)
- Make sure that the Parenteral Nutrition bags do not touch the back wall of the fridge; this may cause them to freeze. You must never use Parenteral Nutrition that has frozen. If this happens please contact the home care company and the hospital team.
- The temperature of the fridge should always be maintained between 2 - 8 degrees Celsius.
- If you are worried that your fridge is not working as it should do, please contact the Home Care Company.
- If the PN has not been stored at the correct temperature you must not use these bags. Please contact the Home Care Company for further PN. If you have no PN to use that night please use the emergency plan. You can also contact the Chelsea and Westminster Nutrition Team for children for advice.
Prior to commencing parenteral nutrition
- You will need to remove the bag of parenteral nutrition from your fridge 4-6 hours before the infusion may begin.
- The best place to keep it until the infusion time is to hang it from your drip stand or lie on a flat surface to warm up.
- It must not be in direct heat (next to radiators etc.) or sunlight.
- Check that the correct name is printed on the PN label and that it is within its expiry date. (If any information is incorrect – contact your home care company and the nutrition team at C&W
- If you have a protective bag, ensure that this is used to cover the PN and protect it.
- Look at the bag carefully for signs of damage and/or leaks.
- Inspect the bag to ensure that there are no particles of cloudy areas. If you are infusing a Vamin bag, this should be a clear yellow colour. If you are infusing a fat bag, this should be a white colour. If you are worried about your PN please contact the home care company and the nutrition team at Chelsea and Westminster.
If the bag of parenteral nutrition does not meet your safety checks, start the checking procedure on another bag. Inform your home care company and the nutrition team at Chelsea and Westminster.
Troubleshooting PN administration
|
Problem |
Possible Cause |
Action |
Prevention |
|
Unable to flush line or line is becoming stiff |
Line partially or fully blocked. |
Check for kinks in the line. Check that the line is not clamped. Check that the clamp site is rotated and has not become stiff. Change the needle free device. Contact the nutrition team at Chelsea and Westminster if not resolved. If outside of hours seek emergency help |
Flushing the central line as soon as the PN has finished. NOT leaving the infusion on KVO. Using the push/pause technique when flushing the central line. |
|
Feeling Unwell +/- temperature. |
Possible central line sepsis. |
Follow the sepsis protocol. |
Follow the rules of Asepsis. |
|
Pump Malfunction |
Malfunction / damage |
Use your second back up pump. Contact the 24hr helpline to arrange collection and replacement. |
Follow pump care instructions. Keep an eye out for the maintenance date – if you see that this is out of date, contact the homecare company. |
|
Air in line |
Pump malfunction. Air In giving set. |
Clamp the central line and stop infusion. Check the line for any air. If no visible air, change the pump and use your back up pump (you can do this without disconnecting). If there is air in the line, prepare your equipment, disconnect and replace with buffer PN bag. If you are concerned that it is a pump malfunction use your backup pump. |
When you remove the PN bag from the fridge, hang it up-right from the stand rather than laid flat. Ensure that there is no air in line before you connect. |
|
No PN available to infuse |
PN bag spoiled during prep. PN bag leaking. PN bag failed your safety checks. Fridge malfunction No PN delivered |
Prepare and Infuse PN Buffer bags**. Use the same infusion volume and ramp up/down times. Notify the Nutrition team at C&W |
Ensure correct procedure used to connect PN. |
Remember to refer to your emergency central line training.
** PN buffer bags are delivered on an as and when basis. You will be delivered a spare lipid and aqueous bag. If you have used this buffer bag please contact us and your HPN coordinate to arrange delivery of more.
Flushing a central line
The central line must be flushed before any PN is administered, to prevent the mixing of incompatible medicines/mixtures and always at the end of the infusion, to maintain patency (preventing blockages).
The central line is flushed by using a prefilled 10ml syringe of 0.9% Saline. We use a technique called the push/pause technique – this helps to clear the tube of any debris and maintain patency.
If the central line is no longer in use, you must flush it once a week.
Locking a central line
Locking a central line is defined as the flush that you lock in the line at the end of the PN infusion (the last flush before clamping and securing the line).
There are a variety of locks. The lock that you use may change over time. A change of line lock will be discussed with you in hospital or in a clinic appointment.
Types of line locks
Hepsal – this is a solution of Heparinised Saline (10IU/ml). Heparin is used to dissolve blood clots. It is thought to help maintain central line patency. This is often used more commonly with our PICC lines due to the smaller size lumen.
Taurolock - The lock solution contains (cyclo)-taurolidine and citrate (4%). (Cyclo)-taurolidine has a broad antimicrobial activity against gram-positive and gram-negative bacteria and fungi. It is thought that locking Taurolock in the line will prevent the formation of bacteria biofilm. Taurolock is used after sepsis episodes.
Antibiotic locks – An antibiotic lock contains a small amount of an antiobiotic (amikacin, vancomycin, gentamicin). An Antibiotic lock is commonly used in the under 5s that seem to experience common bacterial central line sepsis episodes. The Antibiotic lock is not a long term lock.
Flushing solution on discharge - __________________________________
Lock solution on discharge - _____________________________________
Aseptic handwashing
Handwashing and hand hygiene are one most important procedure when looking after someone with a central line.
Before washing your hands remember:
- Nails should be short and well kept
- It is advisable not to wear nail varnish (if you are wearing nail varnish it should not be chipped or flaky)
- Remove rings with stones or ridges on
- Remove watches and bracelets
- Roll up long sleeves (wrists must be clear off all clothing).
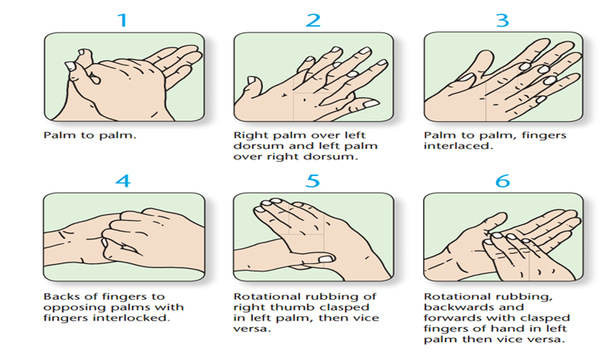
This should last at least 2 minutes.
After washing your hands remember:
- Always rinse from your fingers towards the elbows (so that the dirty water is moving away from your hands)
- Dry your hands with paper towels
- Do not turn off the taps with your clean hands (use your elbows or a paper towel to turn them off)
PN administration technique and CVL care
Procedure for connecting TPN
(All procedures are based on the BAPEN Parenteral Support Catheter Guidelines 2018)
- Identify the key parts
- Ensure no touching of any key parts during the procedure
- Apply alcohol hand rub directly to hands during the procedure if touching any non-sterile contents and/or if there is any risk of contamination
Social handwash
Step 1 - Gather and check equipment
- Bag of parenteral nutrition (PN) (Check PN prescription, integrity of bag & expiry date).
- Trolley/tray.
- Detergent wipes (or paper towel, soap and water).
- 2% CHG & 70% IPA disinfectant wipes.
- Sterile dressing-pack.
- Sterile gloves.
- 10mL pre-filled syringe(s) 0.9% Sodium Chloride for Injection.
- Alcohol hand rub
- Sterile intravenous giving set.
- Infusion pump, stand/rucksack.
Step 2 - Aseptic handwash
Step 3 - Prepare equipment
- Clean & disinfect trolley/tray surface.
- Open sterile dressing pack/towel onto trolley/tray surface to create an aseptic field.
- Open equipment needed onto aseptic field.
- Wearing sterile gloves spike bag of PN and prime giving set.
- Programme pump.
Step 4 - Prepare patient and catheter
- Open sterile towel & place under catheter.
- Remove any outer dressing covering the catheter (if used) & port protector.
Step 5 - Access catheter
- Put on sterile gloves.
- Prime pre-filled syringe.
- Disinfect the Bionector (15 seconds using friction).
- Attach syringe to the Bionector and flush catheter using push pause flushing and positive pressure clamping technique.
- Attach giving set.
Step 6 – Start infusion and secure catheter
- Ensure giving set & catheter clamps are released.
- Start infusion at prescribed rate.
- Remove gloves.
- Secure catheter.
Clear away and social handwash—PN administration technique and CVL Care
Procedure for Disconnecting TPN
(All procedures are based on the BAPEN Parenteral Support Catheter Guidelines 2018)
Key Principles of Care and Management of Central Venous Catheters:
- Identify the key parts
- Ensure no touching of any key parts during the procedure
- Apply alcohol hand rub directly to hands during the procedure if touching any non-sterile contents and/or if there is any risk of contamination
Social Hand wash
Step 1 - Gather and check equipment
- Trolley/tray
- Detergent wipes (or paper towel, soap and water)
- 2% CHG & 70% IPA disinfectant wipes
- Sterile dressing-pack
- Gloves
- 10mL pre-filled syringe(s) 0.9% Sodium Chloride for Injection
- 10ml syringe and filtered needle
- Taurolock locking agent
- Alcohol hand rub
- Parafilm
- Sharps bin
Step 2 - Aseptic handwash
Step 3 - prepare equipment
- Clean & disinfect trolley/tray surface
- Open sterile dressing pack/towel onto trolley/tray surface to create an aseptic field
- Open equipment needed onto aseptic field
Step 4 - Prepare patient and catheter
- Switch off pump and close clamp on giving set
- Clamp catheter
Step 5 – Draw up locking agent
- Put on gloves
- Attach needle to 10ml syringe
- Carefully open up Taurolock ampule (check for expiry date)
- Draw up 0.8mls of Taurolock and remove needle, place back on trolley
- Remove gloves and clean hands
Step 6 - Access catheter
- Put on gloves
- Disconnect giving set from needle-free device
- Disinfect needle free device
- Prime pre-filled syringe(s)
- Attach syringe(s) to needle-free device and flush catheter using push pause flushing and positive pressure clamping technique
- Disconnect syringe and attaché syringe with locking agent. Instil into lumen and clamp under positive pressure
- Attach Parafilm
Step 7 - Secure catheter
- Remove gloves
- Secure catheter
Clear away and social handwash—changing catheter dressing
This procedure should not be incorporated into any other procedure in which the catheter hub is manipulated so keeping the risk of cross contamination to a minimum. Dressings need to be changed every 7 days, if they are soiled or have become loose.
A fabric island type dressing is recommended if there is discharge/infection from the exit site – this will be changed more frequently on advice from the nutrition team.
Social handwash
Step 1 - Gather and check expiry dates of equipment
- Trolley/tray.
- Detergent wipes (or paper towel, soap and water).
- 2% CHG & 70% IPA disinfectant wipes.
- Sterile dressing-pack.
- Sterile Gloves.
- Single use 2% CHG & 70% IPA sponge applicator(s).
- Sterile dressing(s) of choice.
- Alcohol hand rub.
Step 2 - Aseptic handwash
Step 3 - Prepare equipment
- Clean & disinfect trolley/tray surface.
- Open sterile pack/towel and create an aseptic field.
- Open equipment needed onto aseptic field.
Step 4 - Prepare patient and catheter
- Remove existing dressing(s) with apeel
Step 5 - Access catheter
- Put on sterile gloves.
- Disinfect skin with single-use 2% CHG & 70% IPA sponge applicators (using one for the site and the second for the wider skin area (if the line itself is soiled a third is required to clean the line).
- Apply dressing with a secure loop.
Step 6 - Secure catheter
- Remove gloves.
- Secure catheter (as recommended by HPN Centre).
Clear away and social hand wash—Changing Bionector
A Bionector must be changed once a week, for this reason many people choose to do this after they have completed the weekly central line dressing.
Social handwash
Step 1 - Gather and check expiry dates of equipment
- Trolley/tray.
- Detergent wipes.
- 2% CHG & 70% IPA disinfectant wipes.
- Sterile dressing-pack.
- Sterile Gloves.
- Bionector.
- Port Protector.
- Alcohol hand rub.
Step 2 - Aseptic handwash
Step 3 - Prepare equipment
- Clean & disinfect trolley/tray surface.
- Open sterile pack/towel and create an aseptic field.
- Open equipment needed onto aseptic field.
Step 4 - Prepare patient and catheter
- Open sterile dressing towel and place under catheter.
Step 5 - Access catheter
- Put on sterile gloves.
- Disinfect (15 seconds using friction) Bionector.
- Remove Bionector.
- Disinfect the outside of the hub only.
- Replace Bionector swiftly.
- Fasten port protector.
Step 6 - Secure catheter
- Remove gloves.
- Secure catheter.
Clear away and social hand wash—additional activities
Baths/showers
When bathing and showering we would recommend covering the central line dressing – or minimising how wet it gets. If the dressing becomes wet or dislodged during bathing, it must be changed when out of the bath/shower and dry. If bath water is contaminated with poo, please change the Bionector and port protector (if they get wet). If the dressing and central line gets wet during bath time please change dressing immediately.
Swimming
We do not advise letting the central line being submerged and therefore do not recommend swimming in any circumstance
Pets
Pets can be great companions. If you do keep pets in the home it is essential that no Pets are allowed in the child’s bedroom or in the area that the PN procedures are undertaken.
Please always discuss pets with the Nutrition team.
Holidays
Holidays and short breaks are great for families and we like to support these when we can. If you require a change in delivery address or days, you need to give your home care company at least 6 weeks’ notice. The home care company will deliver to any address in the UK and to any port. The PN will be packaged and documents provided for flights and overseas travel.
It is your responsibility, to source a fridge that can be used, as a dedicated PN fridge at your holiday destination.
If you are planning on travelling abroad, it is important that you discuss your travel plans with the Nutrition team before booking. It is important to think about the temperature/heat of your destination, the health care service provision and travel time.
We will provide you with a letter documenting the equipment that you require for travel and a fit to travel document. These documents can only be provided once your plans have been discussed and within a month pre travel.
It is always essential that you have travel insurance for overseas travel.
Remember your hand held letter.
School (training and support)
We will provide or help organise the necessary training for places of education. Depending upon the age and needs of your child, we will provide documents to support an Education Health Care Plan and extra support at school.
Please let us know as soon as you are notified with your child’s school placement, so that we can make contact and start arrangements. If you plan on changing schools please let us know as soon as possible to avoid delays.
Care packages
Continuing care will be discussed prior to your discharge. We will always refer and provide supporting statements for this process.
Children with Disability Teams can be very helpful in some circumstances. Referrals will always be discussed.
Some hospices provide respite and care packages for children requiring PN; we will discuss this as part of the discharge process. Please do not hesitate to contact us for further information.
Activity opportunities
Over the wall is a residential camp facility – an amazing opportunity for young people to take part in a wide range of activities in a safe environment with health professionals to provide care needs. https://www.otw.org.uk/
Please ask the nutrition team for more information.
Home parenteral nutrition training programme
Name of Patient:__________________________
Patient Hosp Number:__________________________
Patient D.O.B:__________________________
Parent/Carer Name:__________________________
Aim: The patient/carer will acquire the knowledge and skills necessary to safely and effectively administer parenteral nutrition and care for the central venous catheter (line).
|
Learning outcome |
COMPETENT SIGN and DATE clearly. |
|
1. To understand why PN is required |
|
|
a. Principles of normal intestinal function |
|
|
b. How gut function has changed |
|
|
c. Understands the potential side effects and complications of PN and can explain how to manage such side effects. |
|
|
2. To understand principles of asepsis |
|
|
a. Washes and dries hands effectively |
|
|
b. Applies hand rub correctly |
|
|
c. Applies gloves correctly |
|
|
d. Prepares area demonstrating knowledge and understanding of ANTT procedure |
|
|
e. Can identify key parts and non-key parts |
|
|
f. Disinfects Bionector for minimum of 30 seconds with pressure and friction |
|
|
3. To safely disconnect and flush line |
|
|
a. Deals appropriately with pump and line at end of infusion |
|
|
b. Prepares syringe with flushing solution correctly |
|
|
c. Flushes line with push-pause technique |
|
|
d. Uses positive pressure clamping technique when disconnecting syringe. |
|
|
e. Prepares and instills line lock correctly (if applicable) |
|
|
f. Applies port protector correctly |
|
|
g. Secures line |
|
|
4. To safely set up PN |
|
|
a. Checks solution correctly |
|
|
b. Primes giving set correctly |
|
|
c. Checks patency of line before connecting infusion |
|
|
d. Uses pump correctly including the correct programming (volume to be infused and hours of infusion including ramp up and ramp down) |
|
|
e. Deals with pump alarms appropriately |
|
|
f. Protects bag from light (where applicable) |
|
|
g. Protects giving set/line connection during infusion (if applicable) |
|
|
h. Can identify and describe the actions required if the PN is not available or if the PN or bag is spoilt or impaired (leaking, contaminated, separated) |
|
|
5. How and when to dress exit site |
|
|
a. Knows when to clean exit site |
|
|
b. Knows what to clean exit site with and method of cleaning |
|
|
c. Suitable dressings to use |
|
|
d. Is able to assess and observe the exit site. Understands when and who to contact for advice. |
|
|
6. How and when to change needle free connector |
|
|
a. Knows how often the Bionector should be routinely changed |
|
|
b. Knows any additional times connector should be changed |
|
|
7. Emergency Pack |
|
|
a. Can identify the key parts included in the emergency pack and where this should be kept. |
|
|
b. Understands the importance of the hand held letter. |
|
|
8. To detect possible infection |
|
|
a. Can identity signs of possible bloodstream infection |
|
|
b. Can identify signs of possible exit site/tunnel infection |
|
|
c. Can demonstrate how to take a temperature using a tempodot device and can articulate when to seek medical attention |
|
|
d. Can identify action to take and point of contact for above |
|
|
9. To prevent air embolism |
|
|
a. Knows how air can enter bloodstream and infusion |
|
|
b. Knows when and how to clamp line |
|
|
c. Knows how to deal with/prevent “air in line” during infusion |
|
|
10. To act appropriately with blocked line |
|
|
a. Knows signs of blockage |
|
|
b. Can identify action to take and point of contact |
|
|
11. To act appropriately with line fracture |
|
|
a. Knows how lines can become fractured |
|
|
b. Can identify signs of catheter fracture |
|
|
c. Knows what to do in case of line fracture |
|
|
d. Can identify point of contact |
|
|
12. Can identify possible line malposition and accidental removal of the line. |
|
|
a. Knows function of cuff and approximate location within skin tunnel |
|
|
b. Understands implication of line malposition |
|
|
c. Can identify actions and contact point required for a dislodged/malpositioned line. |
|
|
d. Can identify actions and contact point required for a line that has been accidentally removed. |
|
|
13. Can recognize signs of possible thrombosis |
|
|
a. Can describe possible signs and symptoms of a central venous catheter related thrombosis |
|
|
b. Can identify action to take and point of contact |
|
|
14. Correct storage of PN, IV fluids |
|
|
a. Can describe how to correctly store PN |
|
|
b. Can read expiry date correctly |
|
|
c. Understands about stock rotation |
|
|
d. Understands importance of cleaning fridge |
|
|
e. Can describe how to correctly store any IV fluids |
|
|
f. Can describe how to safely dispose of any unused prescribed PN/IV fluids or other prescribed medication |
|
|
15. Can identify signs of hypoglycaemia |
|
|
a. Can recognize signs of hypoglycaemia |
|
|
b. Can identify action to take and point of contact |
|
|
c. Discuss actions to take to prevent a hypoglycaemic episode. |
|
|
16. Lifestyle issues |
|
|
a. Knows how to protect line during showering/bathing (as per hospital protocol) |
|
|
b. Knows how to protect the line during swimming and the actions required when getting out of the pool (chlorinated only). |
|
|
c. Pets/animal’s discussed with the patient and family |
|
|
d. Holiday destinations and arrangements discussed. |
|
|
e. Support in education environments discussed. |
|
|
17. To know points of contact at |
|
|
a. Discharging hospital |
|
|
b. Homecare company |
|
|
c. Children’s community nursing team |
|
|
20. Knows about patient support group PINNT (Half) |
|
Parent/carer home parenteral nutrition agreement
Name of Patient:__________________________
Patient Hosp Number:__________________________
Patient D.O.B:__________________________
Patient Consultant:__________________________
My child, ___________________________ has been prescribed Home Parenteral Nutrition (HPN).
I have undertaken the appropriate training for either the administration of HPN and emergency care or stand-alone emergency care. I have had the opportunity to discuss the cautions and risks associated with the use of HPN:
- Central line sepsis and the risks associated with not recognising an infection quickly and acting appropriately (contacting and attending hospital). Any temperature 38 and above must be treated as a central line infection until proved otherwise.
- Re-bound Hypoglycaemia
- Parenteral Nutrition related Liver Disease and the importance of trophic feeds
- Central Line problems and accidents (line displacement, line breakage or damage)
- Central Line access problems (line blockages and replacements)
I have agreed to accept the responsibility and feel competent in the administration of home parenteral nutrition and emergency central line care.
I have agreed to accept the responsibility and feel competent in emergency central line care.
I have been given written guidelines to follow regarding my child’s treatment that I have understood. If I have any queries or do not understand any aspect of my child’s treatment, I will contact the CNS, the Ward, home care team or the on call registrar for advice.
Parent’s Name - Parents Signature –
Registered Nurse - Registered Nurse Signature –
Pharmacist Name - Pharmacist Signature –
Consultants Name - Consultant Signature –
Date -
|
Session |
Supervisor |
Date |
Mother |
Father |
Comments |
|
Aseptic Non-Touch Technique talk and demonstration |
|
|
|
|
|
|
ANTT practice |
|
|
|
|
|
|
Hand washing talk and demonstration |
|
|
|
|
|
|
Hand washing practice |
|
|
|
|
|
|
PN disconnection and flush talk, demonstration and practice |
|
|
|
|
|
|
PN disconnection and flush practice |
|
|
|
|
|
|
Hickman Line Safety Talk |
|
|
|
|
|
|
PN connection and flush talk, practice and demonstration |
|
|
|
|
|
|
Bodyguard Pump |
|
|
|
|
|
|
Session |
Supervisor |
Mother |
Father |
Carer |
Comments |
|
Hickman Line Dressing Change |
|
|
|
|
|
|
Bionector Change |
|
|
|
|
|
|
Session |
Supervisor |
Mother |
Father |
Carer |
Comments |
|
PN disconnection and line flush |
|
|
|
|
|
|
PN connection and line flush |
|
|
|
|
|

