Prevention of Blood Clots following Elective Hip or Knee Replacement Surgery
Prevention of Blood Clots
This leaflet has been produced by the hospital Thrombosis and Thromboprophylaxis Group to help explain how a blood clot can develop and become a deep vein thrombosis (DVT) or a pulmonary embolism (PE). It will also discuss the signs and symptoms of blood clots. We hope it answers some of the questions you may have.
Deep Vein Thrombosis (DVT)
Deep vein thrombosis (DVT) is a common medical condition which occurs when a thrombus (blood clot) forms in a deep vein, usually in the leg or the pelvis. DVT can block off or reduce the flow of blood in the vein.
DVT in the leg or the pelvis can cause pain and swelling in the leg and may result in lifelong disability with painful leg swelling, varicose veins and leg ulcers.
Pulmonary Embolism (PE)
Sometimes the DVT (blood clot) in the leg breaks off and travels to the arteries of the lung where it will cause a pulmonary embolism (PE). PE may cause breathing difficulties and chest pain, and may be fatal.
Venous Thromboembolism (VTE)
DVT and PE are known under the collective term of venous thromboembolism (VTE).
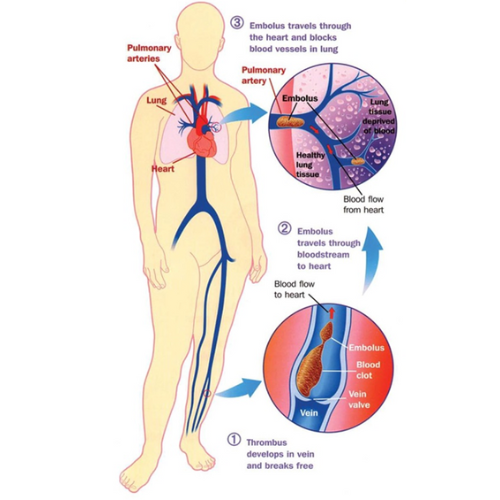
Diagram reproduced with permission of the Thrombosis Research Institute, London UK (2008)
Are you at risk of blood clots?
There are several factors that may increase the chances of developing VTE. If you have more than one of these factors, you may be considered to be at increased risk:
- If you are older than 60 years of age – the risk of VTE is higher the older you are (but young people can also get blood clots)
- If you have previously had DVT or PE, or a close member of your family (parents or brothers and sisters) has had DVT or PE
- Surgery increases the risk of developing blood clots
- If you have certain conditions such as active cancer, heart failure, lung disease or infections (e.g. pneumonia)
- If you are immobile or limited movement
- If you are obese
- If you are pregnant
- If you are taking a certain contraceptive pill or hormone replacement therapy tablets
What can you do to reduce the risk of developing blood clots?
- Keep mobile – move around as much as possible and do some foot exercises.
Here is a simple exercise you can do, even when you are lying in bed, to help your blood to move around your body:
- Lie on your back or sit
- Bend or straighten your ankles quickly
If you keep your knees straight during the exercise you will stretch your calf muscles.

- Take care on journeys – for any long journeys, try to move your legs regularly and take breaks.
- Preventative measures – will be considered if appropriate.
- Compression stockings may be offered in hospital to help the blood flow in your veins
- Hydration – drink plenty of fluids if you are able to
If you have any symptoms of long or excessive bleeding, tell your doctor immediately or
seek urgent medical advice so you can be monitored and have your treatment assessed
Anticoagulant Medication
You may be offered anticoagulant medication known as a ‘blood thinner’ to thin your blood and prevent blood clots if appropriate – take as prescribed and avoid missing doses.
The choice of anticoagulant medication will be based on various factors e.g. kidney function, body weight, other medications that you are taking. Options are:
- Heparin injection is of animal (pig) origin – please discuss with your doctor, nurse or pharmacist if this is a concern to you. You will be shown how to give the injections, and will be provided with a sharps bin to dispose of any needles safely.
- Rivaroxaban tablets (dose is 10mg once a day)
The usual treatment duration is:
- 2 weeks if you have had a knee replacement surgery
- 5 weeks if you have had a hip replacement surgery
Inform your doctor if you are pregnant or breastfeeding.
Like any medicine, anticoagulants may cause side effects, which will vary from person to person. Anticoagulant medication can increase the risk of bleeding and bruising. Please refer to the manufacturers information leaflet for further information.
Tell your healthcare provider about any other medicines you are currently taking, took recently, or intend to start taking before you start this medication.
How will you know if you have DVT or PE?
The symptoms of DVT in the leg include:
- Swelling
- Pain
- Warm skin
- Tenderness
- Redness (particularly at the back of your leg below the knee)
DVT usually (although not always) affects one leg. In some cases, there may be no signs or symptoms of DVT at all in the leg.
The symptoms of PE include:
- Shortness of breath
- Coughing up blood or mucus that contains blood
- Chest pain that is sharp and is worse when taking a deep breath
- Collapse (in severe cases)
Both DVT and PE are serious conditions that require urgent investigation and treatment.
If you suspect you may have DVT or PE, you should seek medical advice immediately either from your GP or nearest A&E (Emergency Department).
Who can you contact for more information?
If you would like any more information or have any questions, please ask a doctor, nurse or pharmacist.
Further information can be found from NHS website (www.nhs.uk) or Thrombosis UK (www.thrombosisuk.org).
Patient Advice and Liaison Service (PALS)
If you have concerns or wish to give feedback about services, your care or treatment, you can contact our PALS service. Send us your comments or suggestions on one of our comment cards, available at our PALS offices on the ground floor of each hospital, or complete the feedback form on our website www.chelwest.nhs.uk/pals.
We value your opinion and invite you to provide us with feedback.
Chelsea and Westminster Hospital
West Middlesex University Hospital

