Advice and information following ankle fracture surgery
This leaflet intends to educate you on the immediate management of your ankle after surgery. It also contains exercises to prevent stiffening of your ankle, once your ankle is no longer immobilised.
Why have I had surgery for my broken ankle?
This surgery is performed after serious ankle fractures that have resulted in the movement of the ankle bones from their ideal position. This could involve one or multiple fractures of the bones around the ankle. Your consultant will inform you of the extent of your injury. During the surgery the bones are repositioned as closely to their original position as possible. This hopefully allows the normal working of the ankle joint. The bones are then held in this place by metalwork. This is necessary to hold the position of the bones whilst healing occurs. How much metalwork you may need depends on the extent of your injury and the way the bone is broken.
What outcome can I expect after my surgery?
The main goal of surgery is to restore the ideal position of the ankle joint and establish the best environment for healing of the bones and tissues. It is important to appreciate that ankle fractures can be serious injuries and that improvement to pain/swelling/function may be on-going for over 12 months after surgery. In order to achieve the best possible outcome following such an injury, you will be referred to physiotherapy who will guide you on your rehabilitation. You should commit regular time to your home physiotherapy exercises.
Treatment plan following surgery
Following your surgery you will be put in a plaster cast or given a boot to support your ankle. You will be told whether or not you can weight bear and will be given specific advice depending on the type of fracture you have. You are likely to require crutches or a frame to help you move safely. You will be given an appointment to return to fracture clinic roughly two weeks after your surgery to ensure the wounds have healed.
Pain and swelling
Pain and swelling will generally be worse in the first two weeks following surgery. It is important to elevate your leg as much as possible during this time to limit the swelling and promote the wounds to heal well. You are also advised to take pain medication.
Ankle pain and swelling may persist for 6-9 months following your injury.
Whilst you are in a plaster cast:
- You will be advised how long the plaster cast needs to stay on and treatment to prevent blood clots or deep vein thrombosis (DVT) will be discussed with you.
- You are encouraged to move your toes and to bend your knee whilst you are in the cast.
- Do not get the cast wet, special covers can be purchased to use whilst washing or bathing; ask staff for more details
- Do not put anything down the cast to scratch, as this can cause an infection if there is any broken skin under the cast.
- Do not cut the cast if it is rubbing or causing discomfort, please contact the plaster room for help (contact details provided later)
Caring for your wound after the plaster cast has been removed
At roughly two weeks after surgery, you will be given an appointment to review the surgical wounds. Once the wound has healed you may get the area wet. Do not pull at scabs or loose skin. Let them fall away naturally. If your wound becomes red, swollen or itchy you need to see a member of the team to ensure there is no infection present. Once fully healed, if you feel the scar is slightly raised or pink then a scar healing gel such as kelo-cote or bio-oil can be used.
Caring for your boot
After your plaster cast is removed, it is highly likely that you will be given a boot to support your ankle. You will be advised about how much weight you can put through your ankle. Remember to wear your boot whenever standing and walking. You can remove the boot to clean the foot and ankle and to facilitate exercises. The boot does not need to be worn at night time.

Initial exercises to do when out of cast
Exercises are important to help restore movement, flexibility and strength to the ankle. A referral will be made for you to see outpatient Musculoskeletal physiotherapy to help guide you through your rehabilitation programme. You should perform these initial exercises 3-4 times a day once you are no longer in a plaster cast.
- Point your foot up and down, repeat this 10 times.

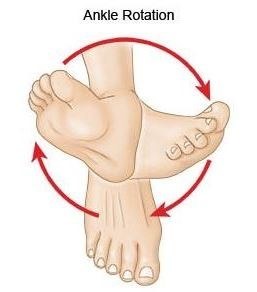
- Make gentle circles with your foot in one direction and then the other direction. Repeat this 10 times.
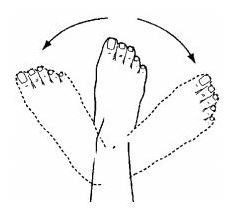
- Move your foot from side to side mimicking a windscreen wiper. Repeat 10 times.
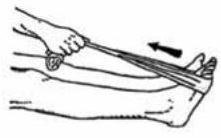
- Sit with your leg straight. Place a towel around your foot and pull back on it until you feel a stretch in your calf. Hold for 30 seconds and repeat 3 times.
Frequently Asked Questions
I am struggling with my boot. What do I do?
The boot has a thicker sole; this can make you feel uneven. Make sure you wear a supportive shoe or trainer on your uninjured foot. This may reduce stress on other joints. If you need more advice contact the Fracture Clinic.
When can I start driving?
You can return to driving when:
- You can walk comfortably and
- You can perform an emergency stop pain free
If you drive an automatic car and you have a boot on your left ankle you may be able to drive provided you meet the criteria above. Always test your ability to drive in a safe environment first.
When can I return to work? How can I get a certificate for work?
The need for a medical certificate will be discussed with you prior to discharge and provided if necessary. Returning to work depends on the type of work you do and on whether you will be able to get to work safely (Please see above for driving advice). Assuming that travel to work is not an issue, office based work can commence almost immediately as long as there are provisions to elevate the foot. For more active duties, it is anticipated that it will be at least 2 months but this will be discussed with you at follow-up with the surgical team.
What do I do with my boot and crutches when I no longer need them?
We are unable to re-use the boot, please dispose of this once you have been told you no longer require it.
Crutches can be returned to the A&E department.
I haven’t received my appointment letter. What do I do?
If you have not received your appointment letter please contact us on
Chelsea Westminster: 020 3315 6666
West Middlesex: 020 8321 5370
How do I contact the Plaster room if I have concerns?
Chelsea Westminster: 020 3315 5204
West Middlesex: 020 8321 5735

