Management of Hallux Limitus
General
Hallux limitus is the name given to osteoarthritis or “wear and tear” of the big toe joint. In a normal joint the surfaces of the bone are covered by cartilage, allowing one surface of the joint to glide smoothly over the other. As the cartilage wears away, the bones rub together results in pain.
As the condition progresses, the body lays down additional bone around the joint margins, which restricts the movement and can obliterate it all together. As the arthritis in the joint gets worse, as shown in the picture below, the treatment options change. In severe cases, conservative care can be less helpful and it is often difficult to save the joint.
Although this condition is progressive the rate of deterioration varies from person to person.
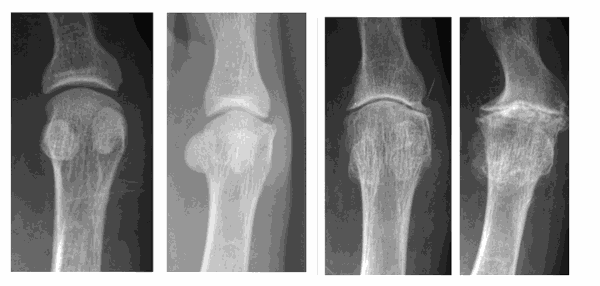
The department has categorised the hallux limitus into mild, moderate and severe.
The pictures below show: 1st = normal – 2nd = mild – 3rd = moderate – 4th = severe hallux limitus.
The cause of osteoarthritis is not clear. Sometimes it is due to a specific joint injury or fracture. However, in most cases we are not sure. Many suggestions have been made, which include poor foot function, an abnormally long first metatarsal, as well as problems in the formation of cartilage. Most people find that the symptoms are made worse by increased activity or wearing shoes with high heels.
Diagnosis
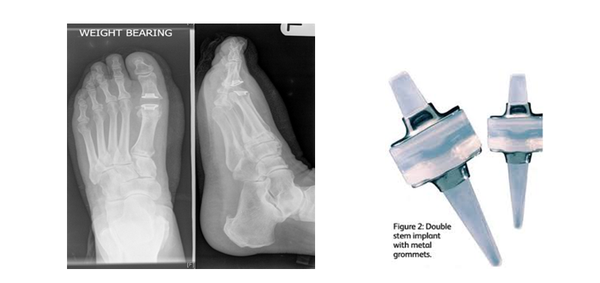
This is made by clinical examination and X-rays. The severity of the joint disease on X-ray can vary from mild to severe, although this does not necessarily correlate directly with the symptoms experienced.
Treatment options
Conservative care
The success of conservative care is based on wearing stiff soled shoes (hiking shoes) or a rocker bottom style of shoe when active. The following treatments may also help when used with these shoes:
- Orthoses
- Anti-inflammatory gel or tablets and analgesics (pain killers)
- Steroid injections

Conservative care is more likely to be successful in the early stages of the condition (mild) However, it is always recommended to try conservative care initially as people with moderate and severe arthritis still report a benefit.
Surgical Management
The surgical management for Hallux Limitus will vary depending on the severity of the arthritis. The surgical options can be divided in two main categories:
- Joint preserving procedures, which aim to extend the life of your joint and reduce symptoms. These procedures should be considered as a stop gap as further surgery is generally required when/if the joint becomes painful again.
- Joint destructive procedures are generally reserved for those with severe arthritis or pain. In some cases, patients may choose this surgical option as they want a definitive solution to their pain early on in the disease process.
The operation
The choice of procedure will depend on the degree of pain, activity levels and radiographic findings. The standard incision is on the side or the top of the 1st metatarsal-phalangeal joint. The incision is normally between 4 and 8 cm in length, depending on the type of procedure you are having. Dissolving sutures are used to close the skin. The operation normally takes about 30 – 60 minutes.
Joint Preserving Procedures
These operations are usually performed on patients who have mild to moderate osteoarthritis in the big toe joint. The operation will hopefully decrease your symptoms and increase your movement for a period of time. If the joint becomes painful in the future, you may require another operation.
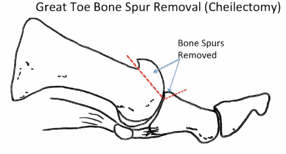
Cheilectomy
This involves cutting away the bony prominences and remodelling the joint. The recovery is relatively short for this procedure and it usually used for mild to moderate joint disease. This procedure is mostly selected when the cartilage is reasonably well preserved and there is a bony bump on top of the metatarsal which restricts the range of motion.
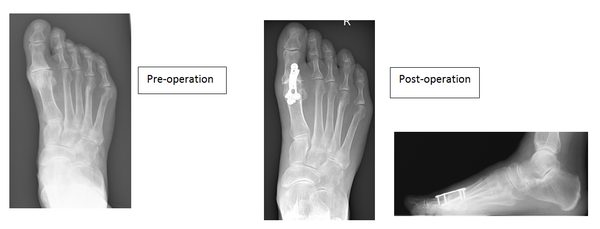
Decompressive metatarsal osteotomy
This involves shortening the metatarsal bone. The bone is cut at an angle and slid back or a small section of bone is removed. In either case fixation is used to maintain the new position whilst the bone heals. This procedure is selected when the 1st metatarsal is longer than the 2nd and when there appears to be adequate cartilage on the joint surfaces to allow movement.
Sesamoidectomy
There are two small bones under the ball of the big toe called sesamoids. Removing these bones can help increase the range of movement and reduce the pain experienced by freeing up the joint. At the same time the bony prominences around the joint are removed. This procedure aims to reduce pain and maintain movement. It is unlikely to resolve the joint pain completely.

Exostectomy
This procedure is used when the joint is not painful but the bony outgrowth results in footwear irritation. The bony growth is removed producing a smooth profile to the joint. There is a risk that the joint may become painful as the range of motion in the joint might increase.

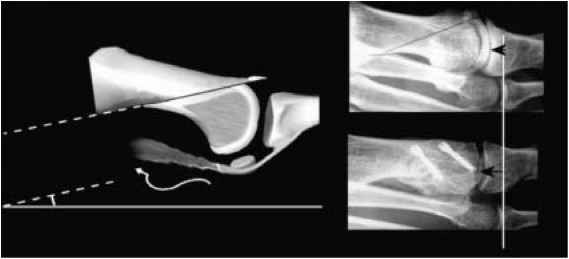
Osteotomy of the proximal phalanx (big toe)
A wedge of bone is removed from the proximal phalanx (bone at the base of the big toe) and gap closed and held with a screw or wire. The procedure elevates the big toe allowing the individual to rock of the toe, this can help reduce pain when walking.
Joint destructive procedures
Joint implant
This operation is recommended for those with moderate to severe degenerative joint disease. The silicone joint implant has a likely life span of 10-15 years. They have been used widely in the UK and US over the past 20 years. The procedure involves making an incision along the top of the big toe joint, removing both sides of the joint and placing a silicone hinged joint in the remaining space. They are not indicated in patients who have an active lifestyle or the under the age of 65 years.
Joint fusion (Arthrodesis)
This operation is generally considered to be the gold standard and is definitive with regard to alleviating pain at the expense of all joint movement.
This is offset by fusing the great toe in slight elevation allowing you to rock through the toe, studies have shown improved weight bearing through the foot following this procedure.
It involves removing both surfaces of the joint and aligning the big toe to allow comfortable walking. The new position is maintained with screws and plates allowing the two bones to join together.
The fixation rarely troubles patients but the plate and screws can be removed if required. The main risk with this procedure is a non-union and the literature suggests around a 6% chance of it happening.
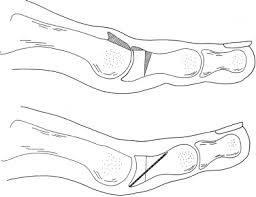
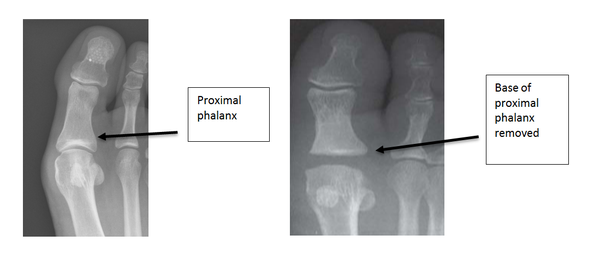
Arthroplasty
This procedure reduces the function of the big toe and can lead to weight transferring to the smaller foot joints. It has the advantage of providing some motion at the joint although the toe post-surgery is significantly shorter. This procedure is generally reserved for patients who have low levels of activity and require a short recovery time. Half of the arthritic joint is removed by resecting the base of the proximal phalanx. The operation should take away the joint pain but can leave the big toe shorter and not as stable on the ground.
Pre and post diagram
Day surgery
You will be admitted to the hospital and discharged on the same day as your operation. On your arrival, you will be shown to the ward and asked to change into a gown. The team will confirm your consent, answer any remaining questions, and mark the surgical site(s).
Anaesthesia
You have the option of having a local (staying awake) or general anaesthetic (going to sleep). In either case the operation is normally carried out as a day case.
General Anaesthesia
On the day of your surgery, prior to having a general anaesthetic, you would be reviewed by the anaesthetic team to ensure that you are fit and well. You will be given all the relevant information on general anaesthesia and the opportunity to ask questions.
Whilst you are asleep we will administer local anaesthetic around your ankle to help reduce post-operative pain. When you wake up in the recovery ward, you will find your foot is numb and this may last between 12 and 36 hours.
Local Anaesthesia
A member of the team will anaesthetise your leg via an injection in the back of your knee (Popliteal block). This will be carried out with adequate time given to allow the local anaesthetic to take effect.
As the anatomy behind the knee varies a little from person to person we use a nerve stimulator to locate the nerves. This sends a small electric current down the needle which stimulates the nerve. This means that the muscles controlled by the nerve begin to contract and relax causing the foot to ‘flick’. This helps us deliver the anaesthetic with precision.
Local anaesthetic at the level of the knee not only blocks sensation but also movement of your foot. This can last between 12 and 36 hrs.
Discharge
Depending on the type of surgery, an Aircast walker will be placed on your leg in the operating theatres or the sandal will be put on by the nurses on the ward. These are removable and should be taken off at rest and the foot and ankle mobilised. You must rest with the leg elevated for the first 48hrs (essential walking only). It is important that you do not interfere with the dressings and keep them dry. You will be shown how to partially weight bear on the foot using crutches (if required).
Post-operative painkillers will be dispensed by the nurses along with your next appointment. You should arrange to go home by car or taxi with an escort.
You should have someone with you for the first 24 hours in case you feel unwell.

Recovery
You must rest with the leg elevated for the first 48 hours (essential walking only). It is important that you do not interfere with the dressings and keep them dry. You can buy a purpose made waterproof cover to keep the leg dry, from your chemist (Limbo M100 above the knee).
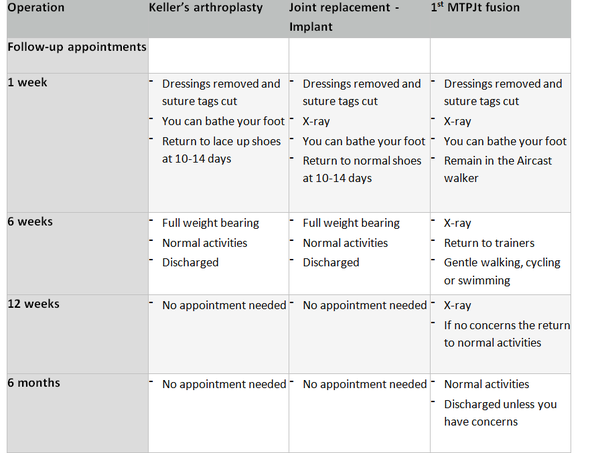
A full recovery takes between seven to twelve months
Reconstructive procedures
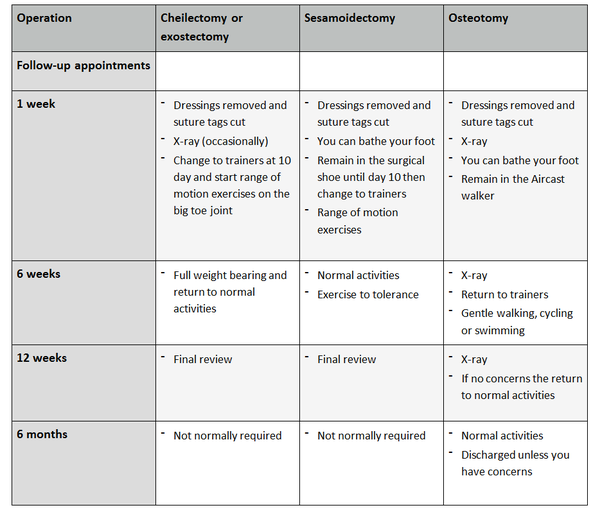
Destructive procedures
Possible complications
Approximately 900 patients undergo foot surgery annually within the Department of Podiatric Surgery at West Middlesex University Hospital. Most patients have an uneventful recovery. Outlined below are the common problems or those rare complications with serious outcomes. In cases where we don’t have accurate audit we have used published results from the podiatric literature. These are accompanied by an asterisk *
- Prolonged swelling taking more than 6 months to resolve occurs 1 in every 500 operations*
- Haematoma – a painful accumulation of blood within the operation site.
- Thick and or sensitive scar.
- Adverse reaction to the post-operative pain killers. 1 in every 50 patients report that the codeine preparations can make them feel sick.*
- Infection of soft tissue. The incidence is 1 in every 83 operations*
- Delayed healing of soft tissue.
- Circulatory impairment with tissue loss occurred in 3 out of 9000 patients over a 10 year period.
- Deep vein thrombosis which can result in a clot in the lung is potentially a life threatening condition. Within the published literature, deep vein thrombosis requiring treatment is 0.3% *
- Chronic pain syndrome, this is where the nervous system dealing with pain over reacts in a prolonged manner often to a minor incident. This normally requires management by specialist in this condition and doesn’t always resolve. This is a rare complication.
Specific complications following a joint replacement
- Rejection of the implant
Specific complications following an osteotomy or joint fusion
- Non-union of bones
- Delayed union (slow healing)
- Fracture
- Joint stiffness
- Fixation irritation
- Further surgery
- Transfer pain
The risk of having a complication can be minimised when the patient and all those concerned with the operation and aftercare work together. This starts with the pre- operative screening and continues through to the rehabilitation exercises.
Pre-operative screening of your health allows us to determine whether you are fit for surgery. It is important that you disclose your full medical history. If there is a query regarding your health, then further investigations or the advice of other surgical and medical specialties will be sought. The surgeon and the theatre team will ensure that the operation is performed effectively and with the minimum of trauma.
You can improve the healing process and reduce the risks of complications by:
- Adhering to the post-operative instructions which include resting and elevating the operated leg. Keeping the wound clean and dry until advised otherwise is essential. Please ask the nurse or Podiatric surgeon if you are unsure.
- Having a healthy diet is important. This provides the nutrition required for healing.
- Smoking is associated with a 20% increased risk of delayed or non-healing of bones.
- Alcohol can interact with the drugs that we will prescribe and in excess can impair wound healing.
- Post-operative mobilisation will be advised. This helps improve the flexibility, strength and stability of your foot
Podiatric surgeons evaluate, diagnose, prevent and treat diseases, disorders and conditions affecting the foot and all associated structures. This is carried out in keeping with the individual’s education, training and experience, in accordance with the ethics of the profession and applicable law.
Podiatric surgeons are not medical doctors.
Podiatric Surgical Training
3 year: Degree in Podiatry (BSc)
2 year: Masters in the theory of podiatric surgery (MSc)
2 year: Surgical training programme
(Podiatric Surgical Trainee)
Final fellowship examinations
(Podiatric Surgeon)
3 year: Specialist training (Podiatric Registrar)
Accreditation with the Faculty of Podiatric Surgery
Consultant Podiatric Surgeon

