Management of nail problems
Ingrown toe nail

An ingrown toenail develops when the sides of the toenail grow into the surrounding skin. The nail curls and pierces the skin, which becomes red, swollen and tender the big toe is often affected, however, any toe can be affected.
What are the symptoms?
- Pain if pressure is placed on the toe
- Swelling and redness at the end of the toe
- An overgrowth of skin around the affected nail
- Bleeding
- Infection – with the presence of pus
Treatment options
Your ingrowing toenail(s) will be treated by one of three methods:
- Partial nail excision with removal of the corresponding nail matrix:
A double longitudinal skin incision is made on the top of your toe through the nail plate and into the soft tissue, in order to expose the base of the nail plate.
- Partial nail avulsion with phenol:
The problematic section of nail is removed. Phenol (a caustic) will be applied to the section of nail bed to stop any new nail growth following removal.
- Total Nail Avulsion:
The nail plate will be removed completely without a skin incision. Phenol (a caustic) will be applied to the entire nail bed to stop any new nail growth.
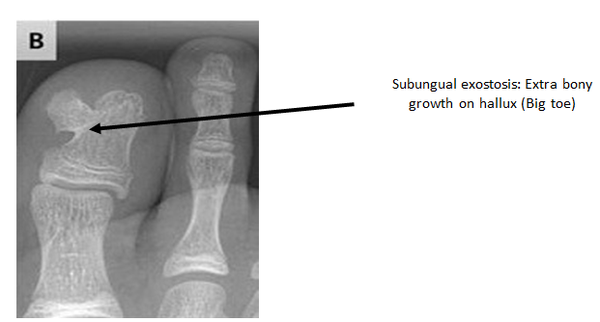
Sub-ungual exostosis
This is a bony overgrowth affecting the tip of the distal phalanx (bone at the end of the toe). If a subungual exostosis is suspected an x-ray is required to exclude or confirm an underlying bony growth.
Subungual exostectomy
The bony prominence will be removed, invariably this will require a section or in some cases all the nail to be removed temporarily. If the nail has been distorted by the exostosis it is unlikely to grow back normally.
Dependant on which procedure, the podiatric surgeon may use stitches to close the skin, which will need to be removed 10-14 days after the operation.
Day Surgery
The operation is carried out as a day case i.e. you will be admitted to the hospital and discharged on the same day. When you arrive at the day surgery unit you will be called into the ward and clerked in by one of the day surgery team.
You will change into a surgery gown and one of the podiatric surgery team will greet you. A member of the team will confirm your consent form and mark the surgical site(s).
Anaesthesia
You may have the option to have a general or local anaesthetic.
General anaesthetic
On the day of surgery, you will be put to sleep by one of the anaesthetic team for the duration of the operation. A member of the team will administer local anaesthetic around your toe to help reduce post-operative pain.
When you wake up in the recovery ward, your toe will be numb and this may last for up to 12 hours.
Local anesthetic
A member of the podiatric surgery team will anaesthetise your toe(s) via two injections into the base of the toe. This will be carried out with adequate time given to allow the local anaesthetic to take effect.
Discharge
Before you leave the hospital you will be given a post-operative shoe, in most cases you do not need crutches. The day surgery team will dispense post-operative pain medication.
You should arrange to go home via car or taxi with an escort. You will need to have someone with you for the first 24 hours in case you feel unwell.
You will be discharged from our department following the surgery. This will mean you will have to attend your GP or practice nurse to have the dressing changed at 1-week and have the sutures removed, if required.
At this stage you may return to a training shoe. Once the dressing and sutures are removed you can wash your foot and gradually increase your activities.
Recovery
You must rest with the leg elevated for the first 48 hours (essential walking only). It is important that you do not interfere with the dressings and keep them dry. You can buy a purpose made waterproof cover to keep the leg dry, from your chemist (Limbo M100 above the knee).
Total nail avulsion with Phenol. The wound may require several further dressing changes and you will be advised to bathe the toe in saltwater (saline) yourself at home. Once out of the post-operative shoe you can drive your car as and when you feel safe.
Possible complications
Approximately 700 patients undergo foot surgery annually within the Department of Podiatric Surgery at West Middlesex University Hospital. Most patients have an uneventful recovery.
Outlined below are the common problems or those rare complications with serious outcomes. In cases where we don’t have accurate audit, we have used published results from the podiatric literature. These are accompanied by an asterisk *
- Regrowth of nail or spicule of nail
- Recurrence of the subungual exostosis
- Thick and or sensitive scar – no audit data is available.
- Adverse reaction to the post-operative pain killers.
- Infection of soft tissue.
- Infection of bone occurred in 3 out of 916 patients.
- Chronic pain syndrome: this is where the nervous system dealing with pain overreacts in a prolonged manner often to a minor incident. This normally requires management by specialists in this condition and doesn’t always resolve. This is a rare complication.
You can improve the healing process and reduce the risks of complications by:
- Adhering to the post-operative instructions which include resting and elevating the operated foot and leg. Keeping the wound clean and dry until advised otherwise is essential. Please ask one of the podiatric team or nurses if you are not sure what to do.
Podiatric surgeons evaluate, diagnose, prevent and treat diseases, disorders and conditions affecting the foot and all associated structures. This is carried out in keeping with the individual’s education, training and experience, in accordance with the ethics of the profession and applicable law.
Podiatric surgeons are not medical doctors.
Podiatric Surgical Training
- 3 year: Degree in Podiatry (BSc)
- 2 year: Masters in podiatric surgery (MSc)
- 2 year: Surgical training programme (Podiatric Surgical Trainee)
Final fellowship examinations (Podiatric Surgeon) - 3 year: Specialist training (Podiatric Registrar)
- Accreditation with the Directorate of Podiatric Surgery
- Consultant Podiatric Surgeon

